
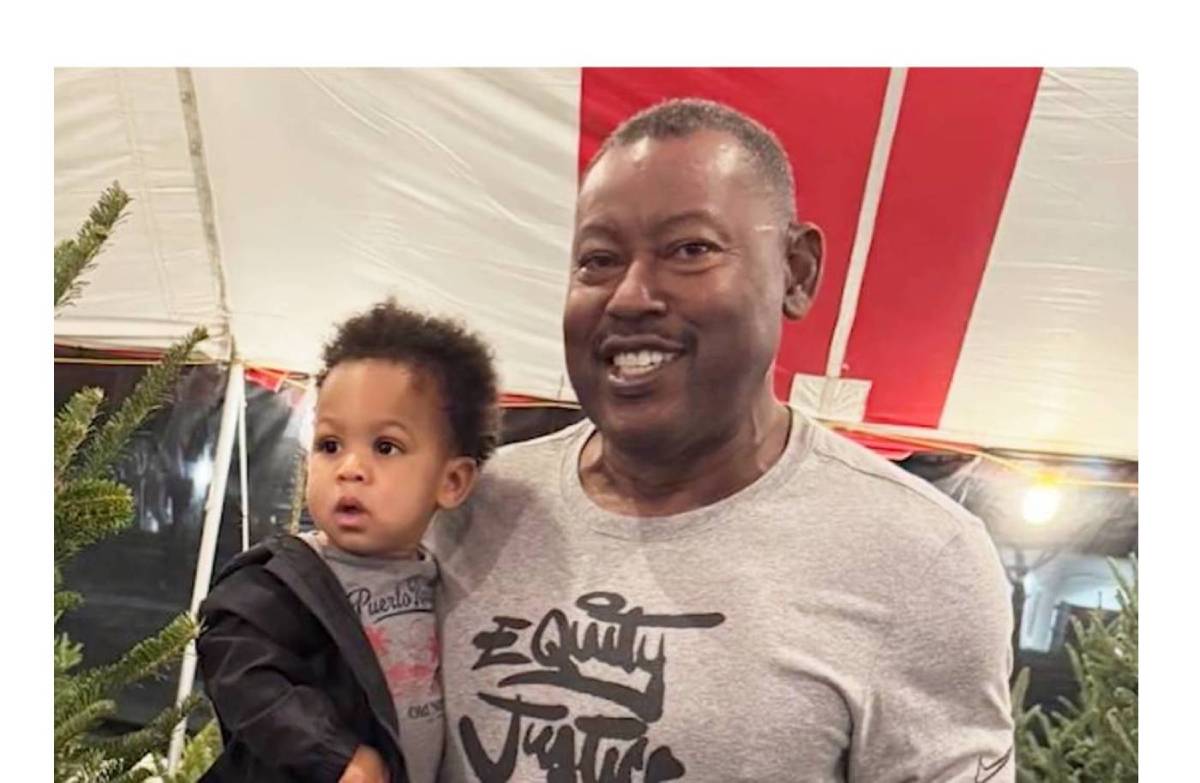
For Marvin Hudson, a dedicated Miami-Dade police officer, retirement in 2018 marked the end of a distinguished career and the beginning of a new chapter with his children and grandchildren. Mr. Hudson wasn’t the type to slow down. He was a lifelong fitness enthusiast, a regular at the gym, and a man who took pride in his physical resilience.
But shortly after hanging up his uniform, Mr. Hudson, now 72, faced an opponent he couldn't arrest or outrun. He was diagnosed with a condition that often hides in plain sight, masking itself behind symptoms that mimic common aging or general heart fatigue. His eventual diagnosis was cardiac amyloidosis, specifically a genetic version known as transthyretin amyloidosis (ATTR).
His story of persistence highlights a critical gap in cardiac care: the difficulty of diagnosing a condition that mimics heart failure and atrial fibrillation (AFib), yet requires a completely different treatment approach.
Today, thanks to advanced care at Baptist Health Miami Cardiac & Vascular Institute, led by Sandra Chaparro, M.D., cardiologist and director of the Institute’s Advanced Heart Failure Program, Mr. Hudson is back to enjoying his busy retirement, proving that a complex diagnosis doesn’t have to mean the end of an active life.

Sandra Viviana Chaparro, MD
“Every time I would see a cardiologist, everything would be fine, and the reason was I had AFib,” Mr. Hudson recalls. “So, if I wasn't in AFib, then I'd get a heart check and everything was fine. I was finally diagnosed with AFib — actually by Miami-Dade Fire Rescue — and that's how the journey began.”
The Fitness Fanatic and the Hidden Symptoms
For most of his life, Mr. Hudson was the picture of health. His colleagues and friends often joked about his strict dietary habits and intense workout regimens. He did everything "right." Yet, he began experiencing heart rhythm issues that didn't align with his lifestyle.
The initial culprit seemed to be AFib, a common irregular heart rhythm. Like many patients who eventually discover they have amyloidosis, Mr. Hudson spent years treating the symptoms rather than the root cause.
This cycle of testing and temporary relief is frustratingly common for amyloidosis patients. Because the condition is a master of disguise, doctors often treat the visible issues—like the arrhythmia—while the underlying protein buildup in the heart muscle continues silently.
The ‘Red Flag’ That Changed Everything
The turning point in Mr. Hudson’s journey didn't happen on a treadmill or in an emergency room, but during a routine consultation. He had already undergone three ablation procedures to correct his AFib, yet his condition was progressing toward congestive heart failure. Something was missing from the puzzle.
It was a small, seemingly unrelated habit that helped crack the case.
“I just happened to be in the doctor's office and I guess I'm a fiddler — and I was fiddling with my hands,” Mr. Hudson says. “The doctor just happened to ask me, 'Do you have carpal tunnel?' And I said, 'Yes, I do.' And he said: I think I'm going to refer you to a specialist just to check to see if you might have this condition.”
That question changed the trajectory of his care. Bilateral carpal tunnel syndrome — numbness or tingling in both hands — is a classic "red flag" for cardiac amyloidosis, yet it is frequently overlooked in heart patients. The condition causes abnormal proteins to fold and deposit in various tissues, including the heart and the ligaments of the wrist.
Following this realization, Mr. Hudson was referred to Sandra Chaparro, M.D., cardiologist and director of the Advanced Heart Failure Program at Baptist Health Miami Cardiac & Vascular Institute. A DNA test confirmed the diagnosis: genetic transthyretin amyloidosis (ATTR).
“It hit me very hard,” Mr. Hudson admits. “I've been fit all my life. And people actually joke about my dietary habits and my workout regimen. It was a pretty devastating diagnosis for me personally, but eventually, I learned to live with it.”
Understanding the ‘Red Flags of Cardiac Amyloidosis’
Dr. Chaparro notes that Mr. Hudson’s case serves as a perfect textbook example of why ATTR is so difficult to catch early, despite the presence of warning signs.
“The unique part of Mr. Hudson's case is that he had all the red flags of cardiac amyloidosis, the typical ones,” Dr. Chaparro explains. “The heart was enlarged. He had arrhythmias … he was being treated for the arrhythmias. But the heart failure continued to progress and he eventually required more support, more specific therapies.”
She emphasizes that while awareness is growing, the delay in diagnosis remains a significant hurdle. When a patient presents with heart failure, physicians usually look for the "usual suspects" like coronary artery disease, valvular disease, or hypertension. When those are ruled out or treated without success, physicians must dig deeper.
“What is important is that whenever you have a diagnosis of heart failure, you always have to look for the underlying cause,” says Dr. Chaparro. “You have to look at the sex, the age, the symptoms, what are the clues, and then try to specify what type of cardiomyopathy that patient has because the treatment is completely different.”
Dr. Chaparro points out specific non-cardiac clues that should trigger a doctor’s suspicion. “When they have bilateral carpal tunnel syndrome or when they have spinal stenosis, when they have kidney disease. Some red flags typical of cardiac amyloidosis.”
A New Era of Treatment
A decade ago, a diagnosis of cardiac amyloidosis offered few avenues for hope. It was often considered a rare, untreatable condition. However, the medical landscape has shifted dramatically in recent years, offering patients like Mr. Hudson a lifeline.
“The therapies for amyloidosis have been developed in the last few years,” Dr. Chaparro notes. “It was until we have one of the medicines that it was released that is a pill once a day that the awareness of this disease increased. The process of the disease was there, but we didn't have the tools to diagnose and we didn't have the therapies to treat these patients. Now, we do have the tools and now we have the therapies.”
Mr. Hudson has experienced this evolution firsthand. Over the past seven years, his treatment regimen has adapted as science has advanced.
“The ATTR treatment has changed over the years,” Mr. Hudson explains. “I started on one drug and it was changed, and then I think three years ago, they added the infusion, and then recently, the infusion changed. So the treatment has changed four times over the past seven years.”
The results speak for themselves. Where he once felt his health slipping away despite his best efforts, he now feels steady and strong. “Before I started treatment, my level of health was declining. Since I started the treatment, everything is stabilized and I'm happy with the direction of the treatment right now.”
The Power of a Collaborative Care Team
Navigating a complex chronic condition requires more than just medicine; it requires a partnership. Mr. Hudson credits his stability to the open, collaborative relationship he shares with Dr. Chaparro and her team. He isn't just a passive recipient of care; he is an active participant in his health management.
“I'm quite satisfied with the team at Baptist Health Miami Cardiac Vascular Institute,” he says. “I love Dr. Chaparro. We have a very collaborative approach to care, and I love that about her. We sit down and we discuss my results, my test results and how things are going, and I love the fact that we can sit down and discuss the care and the direction it's going.”
This partnership is crucial because treating amyloidosis requires precision. As Dr. Chaparro explains, “The medicines are quite specific for amyloidosis, and so it's really important to have the correct diagnosis... You have the heart failures, you have the medicines for heart failure, but you have to have the right diagnosis to start the treatment for amyloidosis.”
Turning a Diagnosis into Advocacy
Marvin Hudson does more than manage his condition — he uses his experience to help others. He understands that if his diagnosis had been delayed any longer, his story might have had a very different ending. He is driven by a desire to ensure others don't miss the signs he eventually found.
“I'm very involved with several organizations, and when I got diagnosed, I did share my story, because it took me a long time to get properly diagnosed,” Mr. Hudson says. “So if anybody was having symptoms similar to mine, I wanted to make them aware of my condition and what the possibilities were. So I do share my story very regularly.”
For Dr. Chaparro, patients like Mr. Hudson validate the importance of constant vigilance in cardiology. “Awareness is really important for the patients or for the medical community to make sure that we diagnose the patients on time now that we have multiple therapies that are quite beneficial.”
Mr. Hudson’s message to other patients, particularly those who might be feeling dismissed or confused by persistent heart issues, is clear and actionable.
“My takeaway is to definitely get tested and stay on top of your treatments, and make it a whole life experience, not only the medication, but your lifestyle, and it all adds up,” he advises. “It all adds up. I think I'm doing very well because I take the whole lifestyle approach to my treatment.”
