A glioblastoma diagnosis can feel overwhelming and the prognosis difficult to hear. But research is accelerating, new treatment approaches are emerging and supportive care options are helping patients and families navigate each step of treatment.
The multidisciplinary brain tumor team of Baptist Health Miami Cancer Institute and Baptist Health Miami Neuroscience Institute delivers advanced therapies tailored to each patient’s specific needs, balancing aggressive treatment with quality of life.

Rupesh Kotecha, M.D.
“Whenever someone is diagnosed with glioblastoma, given how aggressive this tumor is and the number and types of interventions that are required to treat it, we always talk about things like prognosis, longevity, and what a patient's goals or wishes are,” explains Rupesh Kotecha, M.D., chief of radiosurgery and director of the Central Nervous System Metastasis program at Miami Cancer Institute. “We obviously want to provide the patient the best long-term survival possible, but we also want to integrate our efforts into the patient's life.”
That’s what happened for Silvia Fajardo-Hiriart, M.D., a 56-year-old South Florida pediatrician. With aggressive treatment that included three clinical trials, she was able to attend her daughter’s wedding in late April, almost 15 months post-diagnosis. “It was really joyous,” she says. “I can honestly say that it was one of the happiest moments of my life.”

Yazmin Odia, M.D.
Dr. Fajardo-Hiriart continues treatment in an immunotherapy vaccine trial suggested by Yazmin Odia, M.D., chief of neuro-oncology and director of the Brain Tumor Program at Miami Cancer Institute and Baptist Health Miami Neuroscience Institute.
The day after her daughter’s wedding, Dr. Fajardo-Hiriart underwent radiation treatment for a small recurrence on the innovative ZAP-X platform, one of the most advanced forms of stereotactic radiosurgery for treating brain tumors. She is hugely appreciative that her medical team has embraced her desire to fight, despite the grim statistics.
“Probably less than 1 to 5 percent become what they call ‘long-term survivors,’ people who live longer than three years. I was determined to be in that group,” she says. She recalls jokingly telling Dr. Kotecha that she was an overachiever and wanted to be at the top of her class. He knew it was no joke.

Manmeet Ahluwalia, M.D., MBA, FASCO
“He looked at me with a very compassionate but serious tone, and he said, ‘Our team is going to do everything that we can to help you get there,’” she says. “You have no idea how much that meant to me.”
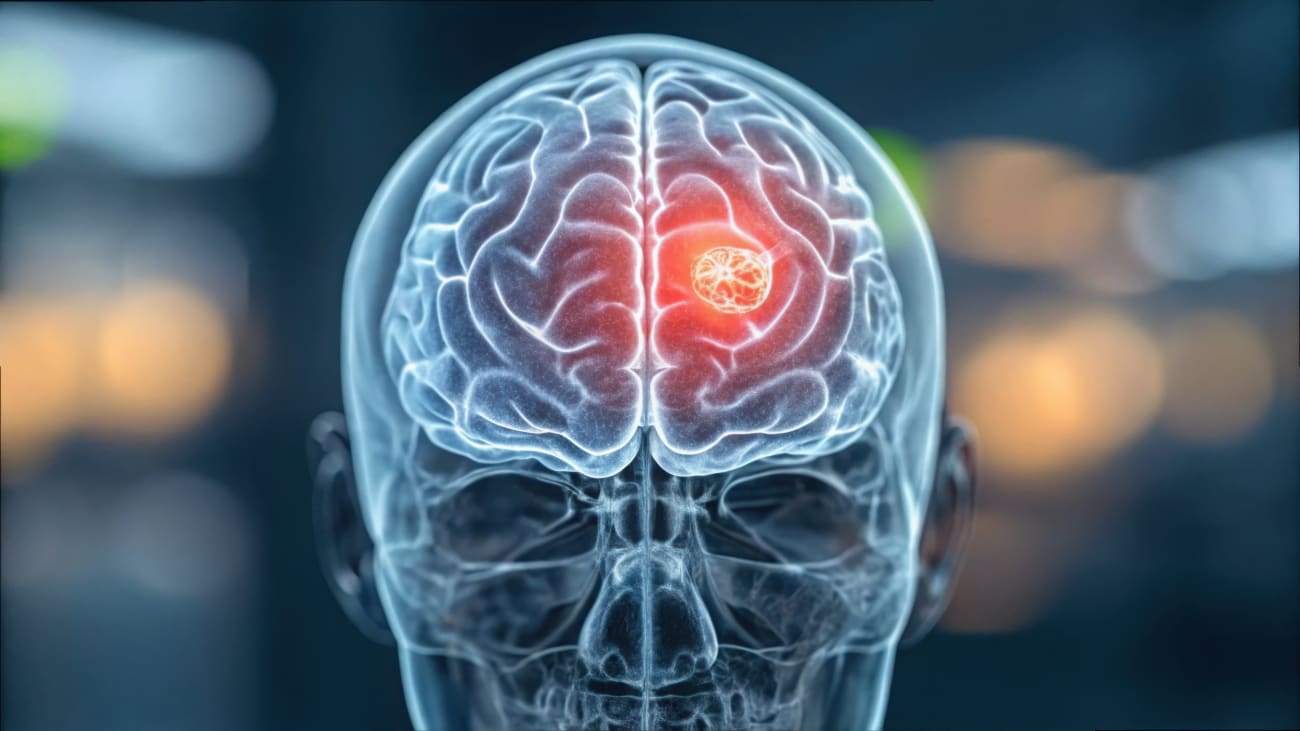
Glioblastoma (sometimes called glioblastoma multiforme or GBM) develops from glial cells —supportive cells in the brain that normally help neurons function properly. It is the most common and aggressive form of malignant brain tumor in adults.
Complete resection is typically not possible because these tumors have finger-like projections that infiltrate nearby brain tissue. A single tumor can contain multiple types of cancer cells with different mutations, making it hard to target effectively with chemotherapy. Moreover, the blood-brain barrier impedes many drugs from reaching the tumor.
Symptoms can vary widely from patient to patient but can include headaches, changes in vision, nausea, disorientation and difficulties speaking. As there is no screening for this type of cancer, by the time symptoms appear, glioblastoma may be advanced
One of the best ways for patients to access cutting-edge treatments is through clinical trials. New immunotherapies, vaccines, targeted drugs and combination therapies are being evaluated across the world. “We really appreciate everything that our patients go through to be able to allow us to treat them, but also to allow us to learn from them,” Dr. Kotecha says.
Miami Cancer Institute researchers have received a $3.4 million R01 grant from the National Institutes of Health and the National Cancer Institute to further research into glioblastoma. The project, “Quantitative Imaging Phenotype Classifier for Distinguishing Radiation Effects from Tumor Recurrence in Glioblastoma,” aims to help distinguish between brain cancer progression and changes caused by the inflammatory process in the brain.
“Research such as this drives the revolutionary change necessary to improve the quality of our patients’ lives and to extend their survival,” says Manmeet Ahluwalia, M.D., MBA, FASCO, the study’s co-principal investigator. He holds the Fernandez Family Foundation Endowed Chair in Cancer Research, as well as serving as chief of medical oncology, chief scientific officer and deputy director of Miami Cancer Institute and Baptist Health Cancer Care.
Dr. Ahluwalia is also leading a multicenter study, “Blood-Brain Barrier Disruption (BBBD) for Liquid Biopsy in Subjects with Glioblastoma Brain Tumors.” The trial uses low-intensity focused ultrasound to perform a liquid biopsy of a brain tumor. During the procedure, the blood-brain barrier is temporarily disrupted, allowing tumor DNA to leak into the bloodstream, where it can be detected in a blood test.

Vitaly Siomin, MD
Dr. Kotecha is leading a phase II trial, “Testing the Addition of Immune Therapy Drugs, Tocilizumab and Atezolizumab, to Radiation Therapy for Recurrent Glioblastoma.” Physicians hope that the combination of immunotherapy medications and radiation therapy will improve the body’s ability to use its immune system and attack the cancer cells, helping to shrink or to stabilize the cancer better than radiation therapy alone in patients with recurrent glioblastoma.
Dr. Odia is principal investigator in three phase III trial exploring medication combinations for glioblastoma. To learn more about clinical trials available at Baptist Health, click here.
“Seeking care at a comprehensive centers like Miami Cancer Institute and Miami Neuroscience Institute can provide access to neurosurgeons who specialize in brain tumors, multidisciplinary tumor boards that review complex cases, advanced treatment options, clinical trials and comprehensive support services,” says Vitaly Siomin , M.D., director of cerebrovascular surgery and co-director of skull base surgery at Miami Neuroscience Institute. “As a neurosurgeon, I believe a team-based approach — one that includes a neuro-oncologist and a medical oncologist who treat only brain tumor patients every day — is invaluable.”
